15 Jun Spike in hepatitis C cases among injection drug users alarming to health experts
Health experts are concerned about a potential HIV outbreak among opioid users on Long Island amid a shift in recent years from prescription drugs such as OxyContin to injectable heroin and fentanyl.
A worrying sign, they say, is the alarmingly high number of injection drug users with hepatitis C, which is spread by some of the same behaviors that lead to HIV infection.
Spikes in HIV cases among injection drug users have occurred in other states. The Massachusetts Public Health Department in February sent out an advisory declaring a “statewide outbreak of HIV infection in persons who inject drugs,” and a small Indiana county is still reeling over an outbreak that led to 215 newly diagnosed HIV infections in less than 2 1/2 years.
On Long Island, “Everybody is just on pins and needles,” said Dr. Joseph McGowan, medical director of Northwell Health’s Center for AIDS Research and Treatment in Manhasset. “We’re waiting for something bad to happen.”
During the 1980s and 1990s, hundreds of injection-drug users every year were being diagnosed with AIDS on Long Island. HIV, the virus that causes AIDS, is easily spread through blood on shared contaminated needles, and to a lesser extent from “cookers” and water used to convert opioids into an injectable form. Multiple users sometimes dip contaminated needles into the same bottle-cap-like cooker and water, often not knowing they are putting themselves at risk for HIV and hepatitis C, said Tina Wolf, executive director of Community Action for Social Justice, which distributes clean syringes to opioid users throughout Long Island.
About two-thirds of that program’s new clients said they have hepatitis C, she said. Hepatitis C is far easier to contract than HIV from contaminated equipment, and it’s a sign of risky behavior, said Don Des Jarlais, a professor of epidemiology at New York University who is affiliated with NYU’s Center for Drug Use and HIV/HCV (Hepatitis C) Research.
HIV spread rapidly among injection drug users in the 1980s and 1990s. Nationally, more than 250,000 injection drug users died of AIDS from the 1980s through 2016, according to the U.S. Centers for Disease Control and Prevention. Some of those users also were men who had sex with men.
HIV-positive people today survive far longer on average than in the first decades of the epidemic, because of a combination of medications that can make the amount of HIV in the blood so low that it is undetectable, and that has made the disease a manageable, chronic condition for those in treatment.
From 1982 to 1999, before many of these medical advances, nearly 2,900 injection drug users on Long Island were diagnosed with AIDS — more than 45 percent of all AIDS diagnoses Islandwide, according to CDC data.
Those numbers plummeted in recent years. There were 11 new HIV diagnoses among injection drug users on Long Island in 2017, less than 6 percent of all new HIV cases, according to New York State Department of Health data.
The number of new HIV diagnoses among drug users statewide also fell. The key reasons, experts said, are clean-syringe programs, a 2000 state law that allows syringe sales without prescriptions and HIV education of drug users.
“In the 90s, before we legally authorized and funded the syringe exchanges in New York City, we were seeing about 4,000 new cases a year of HIV infection among people who inject,” Des Jarlais said. “And now we’re down to about 40 new cases per year.”
Multiple studies show that syringe exchange programs reduce HIV infection without increasing drug use, he said.
Some syringe-exchange programs in the state have fixed locations and hours. On Long Island, Community Action delivers syringes — and picks up special plastic containers with used syringes — wherever people want, usually at their homes, Wolf said.
In 2012, Wolf started a syringe-exchange program for the now-defunct Long Island Minority AIDS Coalition, with a van distributing needles from fixed locations. Relatively few people participated, largely because of limited opening hours, transportation issues and a reluctance by users to be publicly seen obtaining needles, Wolf said. Community opposition blocked a proposed site in Freeport. She co-founded Community Action in 2013.
Since then, the number of people on Long Island who inject opioids has increased, largely because of more aggressive crackdowns on doctors who overprescribe opioids and a 2013 state law that imposed more stringent monitoring of opioid prescriptions, said Jeffrey Reynolds, president and CEO of the Mineola-based Family and Children’s Association. That led to more people who “go straight to heroin and fentanyl” without ever using pills, he said.
The number of Long Islanders who inject opioids is unknown. More than 6,500 people who inject opioids sought treatment in 2018 at a state-certified center, according to the state Office of Alcoholism and Substance Abuse Services.
Community Action serves about 1,200 clients each year, Wolf said. Some users are wary of the syringe exchange, thinking it’s a police setup, and they don’t realize possession of syringes is legal for those in the program, she said. The group gives clients a plastic “NYS Authorized Syringe Exchange Program” identification card.
Almost all of the more than $940,000 in annual funding for the program is from the state Department of Health, department officials said.
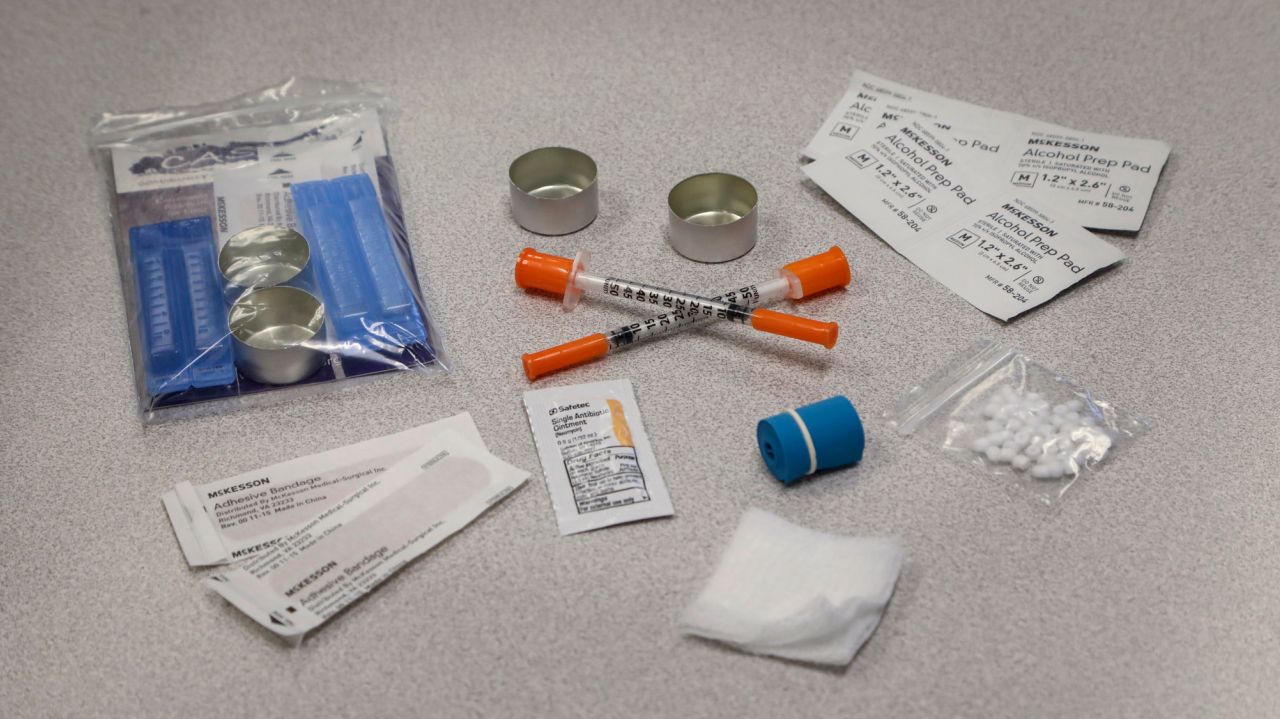
The group’s five employees deliver as many syringes as users want, along with new cookers, fresh water, the anti-overdose drug Narcan and condoms. They also educate users on how to avoid contracting HIV and hepatitis C.
As use of the synthetic opioid fentanyl has risen, so has the need for clean syringes, because the high from fentanyl doesn’t last as long, leading to more frequent injections, Wolf said.
Most users know that needle-sharing can transmit HIV, but, Wolf said, “I’ve enrolled people who have said, ‘Oh, you can still get HIV?’ ”
Even people who know they shouldn’t share syringes sometimes do if the alternative is a wrenching drug withdrawal. “They’re dope sick, they’ve got drugs, there’s one needle, and there’s more than one person,” she said.
With hepatitis C so common among users, “I’m kind of waiting for the dam to break,” Wolf said. People who are part of drug-using networks generally trust those with whom they inject, so “they don’t necessarily take the same precautions they would otherwise. The problem is once one person goes outside of that risk network, potentially everybody is in danger.”
Scott County, Indiana, illustrates how quickly HIV can spread. Between late 2014 and early 2017, 215 injection-drug users — nearly 1 percent of the population of the small county — were diagnosed with HIV infection.
A 2018 Yale University study concluded that the lack of a syringe-exchange program — despite pleas starting in 2008 to establish one — and the closure of the area’s only HIV testing site after state budget cuts helped fuel the outbreak. Under pressure, then-Gov. Mike Pence authorized a syringe-exchange program in Scott in 2015, after the scale of the HIV outbreak became clear.
In Massachusetts, there have been HIV outbreaks in the last few years in Boston, Worchester and — in by far the largest “cluster” — in the small cities of Lowell and Lawrence, where there have been 166 new HIV diagnoses among injection-drug users between 2015 and this month, said Kevin Cranston, director of the Massachusetts Bureau of Infectious Disease and Laboratory Sciences.
Syringe-exchange programs began in Lawrence and Lowell in 2017 and 2018, and the state and local nonprofits ramped up HIV education, HIV testing and other efforts, Cranston said.
The two cities may have been hit so hard because fentanyl — with the typically higher number of injections — may have arrived there before elsewhere in the state, he said.
Reynolds said outbreaks elsewhere are a cautionary tale for Long Island.
“All you need are one or two HIV-positive cases and it could potentially spread really, really quickly,” he said.
DECLINE IN HIV CASES
The number of HIV and AIDS cases in Nassau and Suffolk counties among injection drug users has declined sharply since the 1990s.
AIDS diagnoses of injection drug users on Long Island
1992: 326
1993: 330
1982-1999: 2,915
HIV-infection diagnoses of injection drug users
2017: 11
The figures in the 1980s and 1990s are for AIDS cases. The 2017 number is for HIV. The state did not begin to track HIV diagnoses until 2000. It typically takes years for untreated HIV infection to develop into AIDS. The 2017 numbers do not include incarcerated people.
Between 1982 and 1999, 365 of the injection drug users who were diagnosed with AIDS also were gay or bisexual men. In 2017, 5 of the 11 HIV diagnoses were men who have sex with men.
SOURCES: U.S. Centers for Disease Control and Prevention, New York State Department of Health
[ad_2]
Source link



No Comments